Marie-Louise ConnollyBBC News NI health correspondent
 BBC
BBCA retired surgeon has said there was a “toxic and unnerving” environment within the Belfast Health Trust intensified by “secret files” being kept on staff.
In recent years, staff have reported alleged bullying and harassment.
BBC News NI can also reveal that it understands the trust has paid out millions in public money in legal cases to staff who allege victimisation and career damage after whistleblowing.
In a statement, the Belfast Trust said it was “regrettable” that issues with staff ended up as High Court or industrial tribunal cases and it was “deeply disappointing” to read the concerns of former employees.
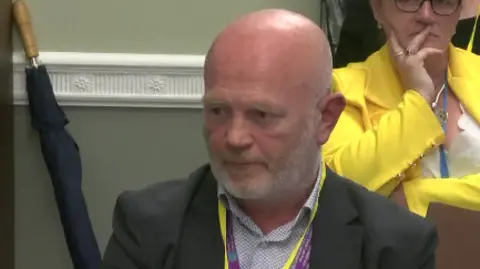
Dr Kieran McManus, who worked in the Belfast Trust for almost 40 years, is the first medical consultant to publicly speak out about the alleged bullying and harassment.
He says medics continue to feel like they are “walking on eggshells” and are often too afraid to raise patient safety concerns.
Dr McManus, who left the trust in 2023, said: “You are working under a degree of oppression and that makes you risk averse – the worst thing is a surgeon who is risk averse and who won’t take risks on a patient’s behalf.
“You are afraid to ask questions, you are afraid to make eye contact with people in corridors.”
Multiple sources who approached the BBC described feeling “paranoid”, “insecure”, “isolated” and “mentally unwell” after learning that “secret files” were being kept on them.
A common thread that links most of these cases is that the people involved blew the whistle on patient safety or had defended colleagues who had done so.
Belfast is the largest of Northern Ireland’s five health trusts, and covers the Royal Victoria, Mater, Belfast City and children’s hospitals.
It is understood about a dozen cases have been taken by Belfast Trust staff over their alleged experiences following whistleblowing, including several cases which are still ongoing.
Money, which includes at least two seven figure sums, was paid to settle High Court and industrial tribunal cases taken by senior medics against the health trust in the past seven years, the BBC understands.
Dr McManus said the hidden costs to investigations are “phenomenal”, as they often result in locums (agency staff) being brought in when doctors have to temporarily step aside.
In its statement, the Belfast Trust said it had paid £1.3m in settlement sums to former employees – BBC sources however say the sum is double that.
The trust said it recognised the right to act under whistleblowing guidelines, adding: “The Belfast Trust actively listens and responds to the concerns expressed by former staff members, and we are committed to learning from their experiences.
“All staff should feel safe, respected and supported within their workplace.”
‘Secret files’
Dr McManus said he was cleared after a five-year investigation which included a trainee accusing him of bullying.
Separately, he had raised issues over patient safety.
During this time, he believes a “secret file” was kept on him.
He is critical of the “lack of confidentiality” over his investigation and the toll it took on his family.
BBC sources said there remains a “fear factor” about what has been happening in the trust, and people are afraid of being targeted for speaking out.
A union representing doctors says at one stage there were about 120 so-called secret files on staff.
They were kept in a filing cabinet in an office not related to the trust’s human resources (HR) department – a practice which constituted maladministration, the union says.
BBC News NI has spoken to multiple people who have left the Belfast Trust following allegations of bullying and harassment made by them and about them.
They include former directors and front-line medical staff who are either working elsewhere or retired.
Except for Dr McManus, none of these people were prepared to be formally interviewed.
Dr McManus said many staff members felt they were “being watched” and believed trainees were often used to gather information which would end up in a file.
Many doctors were unaware there was a separate file on them outside of normal employment documents.
Up to 8% of doctors working for the trust have had files kept on them, the union says. It is not clear if those files have been destroyed.
Giving evidence to Stormont’s Health Committee in June, the trust’s medical director, Dr Chris Hagan, confirmed that when he took up the post in 2020 there were about 100 files on doctors. There are now about 15, he said.
He described the files as being part of the trust’s MHPS (Maintaining High Professional Standards) process, which manages concerns about misconduct, incapability, or poor performance of staff.
“We went from about 7-8% of the medical workforce in some sort of process to less than 1%,” said Dr Hagan.
“There is no-one in a formal MHPS process at the minute,” he told the committee.
He said the trust had about 1,400 permanent medical staff and up to 700 trainees.
Dr McManus, who came from Australia to work in the Belfast Trust in 1979, said authorities in Northern Ireland do not know how to handle a whistleblowing culture.
“My process went on for five years – it even continued after I retired,” he said.
“I was luckier than some of my colleagues who I know have had their lives ruined by these legal processes.”
He said the complaints that lead to an MHPS investigation never exist in a vacuum but are usually the consequence of a dysfunctional system, including personal conflicts.
Whistleblowing
A trade union which represents hospital doctors says whistleblowers in the trust have been subjected to “unwarranted scrutiny” and suffered a “detrimental impact on their career”.
The HCSA (Hospital Consultants and Specialists Association) has raised concerns with senior managers at the trust over the treatment of its members and patient safety.
The BBC has seen several concerns raised by the union to the Belfast Trust and the Department of Health in 2023 and 2024 based on evidence from members.
The document alleges there were “attempts to silence and to take detrimental action against individuals who raised patient safety concerns”.
The HCSA says the evidence provided by medics revealed “tactics to suppress truth, silence legitimate criticism and cover up impropriety”.
Sources have told the BBC that some doctors who settled their cases have signed Non-Disclosure Agreements.
The Belfast Trust said that the Medical Director’s Office is supported by both “internal and external advisers to ensure all decisions and next steps are fair and proportionate.”
 Getty Images
Getty ImagesFollowing several extensive independent reports into health trust culture and allegations of bullying and harassment, a new chief executive has been appointed.
The health minister said Jennifer Welsh’s appointment came at a time of “immense challenge and opportunity”.
The trust has recently begun civility training courses for employees.
Those who spoke to BBC News NI said this is all a matter of public interest as it involves public money and impacts on patients when doctors aren’t working to their full potential.
The Department of Health said it was never desirable for public money to be used for legal or financial settlements.
“The department recognises the vital importance of whistleblowing in safeguarding patient safety and promoting transparency. It continues to support trusts in strengthening their whistleblowing procedures and fostering a culture where staff feel safe and supported when raising concerns.”
The department said there was an ongoing review aimed at tackling poor culture and behaviours within the Belfast Trust.