Unitedhealth Group (NYSE:) is a bellwether for the health insurance industry. The company symbolized the flaws in managed care organizations (MCOs) in the medical sector after its UnitedHealthcare CEO was assassinated in December 2024. Allegations of 32% medical claims denial rates, while earnings continued to break records, highlighted its “profits over patients” reputation.
UnitedHealth has since stated that they pay about 90% of medical claims upon submission and elaborated that only around 0.5% of submitted claims require further review.
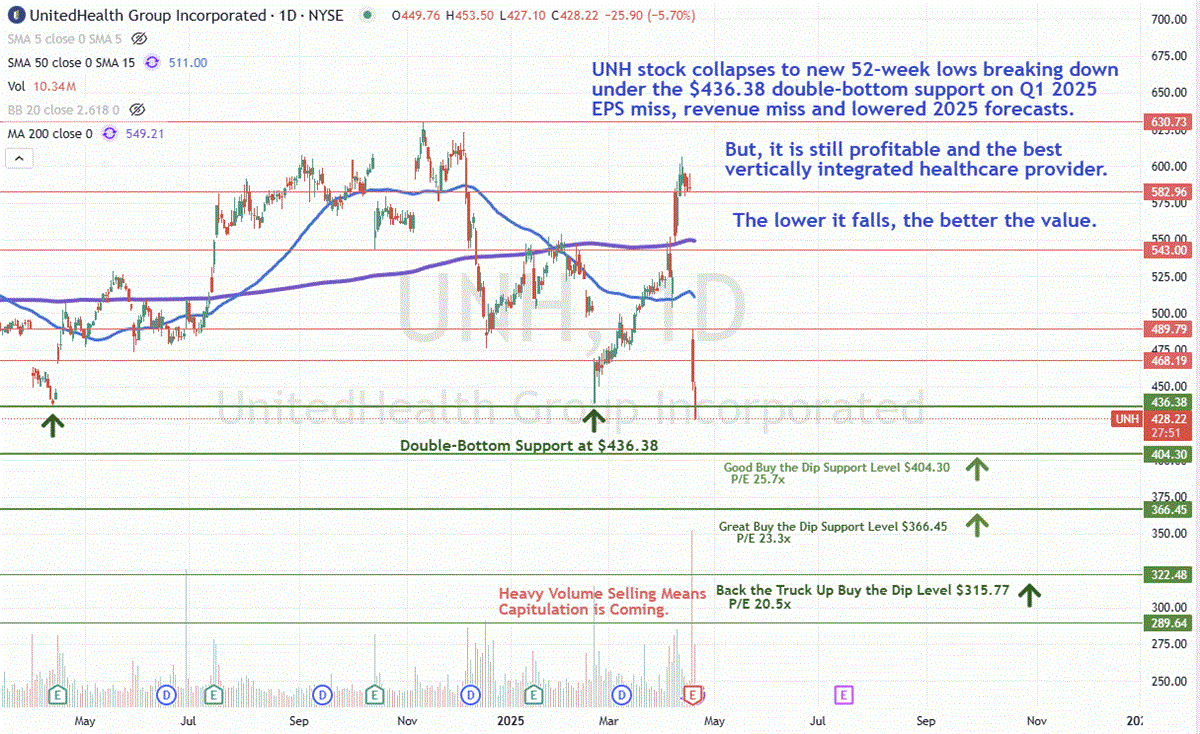
The company’s stock had been recovering off its double-bottom support levels around $435, rebounding as high as $606.36 on April 11, 2025, ahead of its first quarter 2025 earnings report.
Indeed, it rose from a pariah back to pole position as health insurance stocks were seen as recession-resistant safe havens against import tariffs. Peers like Humana (NYSE:) and CVS Health (NYSE:) also enjoyed the money flow surge.
Even as the sentiment shifts negative again for health insurers due to rising medical utilization and medical costs, UnitedHealthcare remains the best house in a rough neighborhood because of its diversified business model as a vertically integrated healthcare organization.
FQ1 2025 Missed Consensus Analyst Estimates, But Vertical Integration Pays Off
UnitedHealth posted fiscal first quarter 2025 earnings per share (EPS) of $7.20, missing consensus estimates by 9 cents. Revenues grew 9.8% year-over-year (YOY) to $109.58 billion but still fell short of the $111.58 billion consensus analyst estimates by $2 billion. Its customers grew to 780,000 year-to-date.
UnitedHealth’s Optum Subsidiary Generated 42% of the Operating Profits
Optum Health added 650,000 new value-based care patients in the quarter. Optum Health is the medical services provider subsidiary of UnitedHealth Group, which bills its UnitedHealthcare insurance subsidiary for claims reimbursements. This is what makes UnitedHealth Group a vertically integrated healthcare organization. The Optum subsidiary reported Q1 revenue of $63.9 billion, up 4.4% YOY. Optum’s operating income was $3.9 billion, which was 42% of the total company-wide operating income of $9.2 billion.
MCR at 84.8% Is One of the Industry’s Highest
A truly notable metric was its extremely low medical care ratio (MCR), also referred to as the medical benefits ratio (MBR) or medical loss ratio (MLR), which is the percentage of health insurance premiums that are paid out for medical services. While 80% is the minimal federally mandated MLR, the measure of cost containment and profitability is usually determined by a lower MLR. While UnitedHealth’s 84.8% MCR upticked slightly from 84.3% in Q1 2024, it is still the second lowest MCR among the largest health insurers.
Medicare Advantage Costs Triggered Downside Guidance and 20% Stock Haircut
UnitedHealth surprised investors with its lowered earnings guidance. For the fiscal full year 2025, the company cut its EPS to $26.00 to $26.50, with a midpoint of $26.25 versus $29.72 consensus analyst estimates. The cut was primarily due to rising medical care activity, with its Medicare Advantage (MA) plan members far surpassing earlier forecasts. This led to a full-year 2025 MCR guidance to rise to 87.5%, up from the previous guidance of 86.5%. Higher MCR means smaller profits.
Not All Is Lost; Management Has a Plan
CEO Andrew Witty still expects strong growth across its businesses. Weakness in Optum Health would be offset by strength in OptumRx. However, Witty acknowledged the unusual and unacceptable underperformance. He reminded investors that UnitedHealth Insurance and Optum are distinct business models.
MA care activity in Q1 increased at twice the rate, consistent with utilization in 2024. Unanticipated changes to its Optum Medicare membership impact 2025 revenue. Optum experienced unexpectedly low patient engagement in 2024 but then saw it surge starting in 2025. Additionally, the CMS risk model impacted new and existing complex patients more.
HouseCalls Program Will Improve Engagements and Outcomes
The Center for Medicare and Medicaid Services (CMS) announced a 5.06% increase to its MA plan reimbursements for 2026, which could be a positive catalyst that is still too early to factor in. Its HouseCalls program is only available to MA plan members and provides thorough home clinical visits at no additional cost to members.
UnitedHealthcare will adapt and improve more effectively, increasing engagement with members at home after post-inpatient discharge. Consistent engagement has proven to be key to better outcomes. MA plan membership is expected to grow by 800,000 more members in 2025.
Witty is doubling down on the virtues of MA: “Further, Medicare Advantage also costs taxpayers less and delivers more to seniors than the fee-for-service Medicare, especially in value-based care arrangements. An essential approach in achieving both health outcomes and lower costs is ensuring people get the care they need when and where they need it.”
UNH Forming Buy the Dip Opportunities Here
UNH stock fell through the double-bottom support level at $436.38, marking a new 52-week low. The maximum four-year price-earnings (P/E) ratio was 37.6x in December 2023. UNH is trading at the lowest price-earnings level since September 2021 at 27.6x.
Three distinctive buy-the-dip levels depend on your preference and timing:
$404.30 is a “good” buy the dip price level as the P/E would fall to 25.7x.
$366.45 is a “great” buy the dip level as the P/E would fall to 23.3x.
$322.48 is a “back the truck up” buy the dip level as the P/E would fall to a bargain 20.5x.
